FCS Editor’s Note: The week before Tulsans were issued the “shelter in place” order, Family & Children’s Services (FCS) had already deployed remote operations, providing care and treatment for patients with mental illness. In addition, FCS had supplied crisis and medical staff with personal protective equipment. That same week, Mental Health Weekly interviewed FCS’s CEO Gail Lapidus about increased mental health disorders, prolonged isolation, hospital bed adequacy, lost revenue and staff safety in the wake of the COVID‐19 epidemic.
COVID‐19 outbreak represents a new way of mental health service delivery

by Valerie A. Canady,
Mental Health Weekly,
March 20, 2020
“Mental health centers are going to be concerned with lost revenue, increased costs and the use of telehealth on certain platforms. We have been gearing up for telehealth for quite some time. – Gail Lapidus
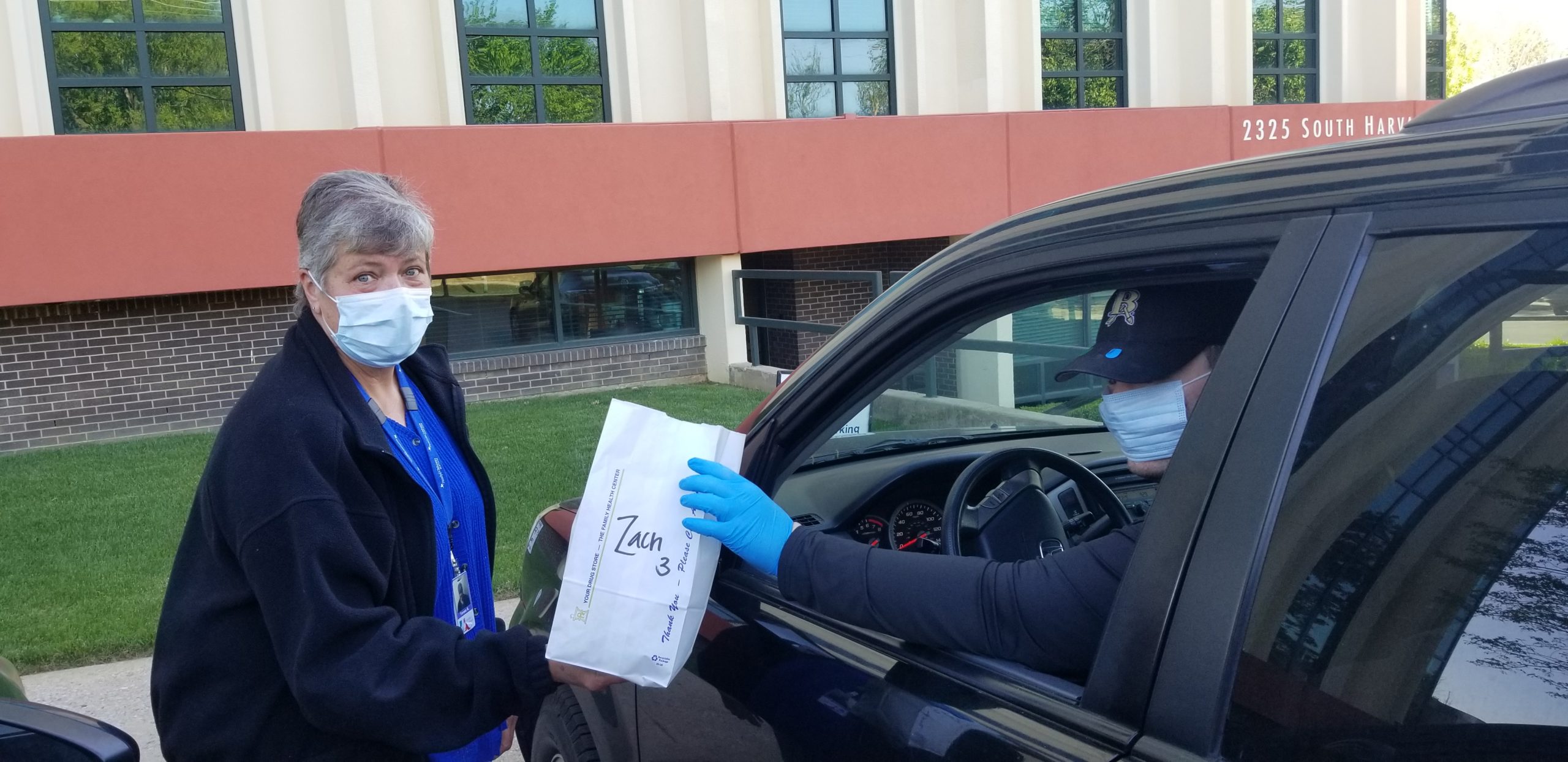
“We’ve moved to virtually calling clients and scheduling appointments. We’re providing care to the community and doing what we can to decrease the risk of exposure. In a pinch, we were able to pivot rapidly to adapt to the pandemic crisis, keeping our staff safe and keeping our community served. We are committed to our clients.” – Gail Lapidus
“We’ve had to rely on the gifts and talents of our IT department. They played a big role in helping with the transition. Other services, like bars, restaurants and some businesses, can close their doors, but we can’t.” – Gail Lapidus
Staying in business
How will mental health centers stay in business? In addition to ensuring staff are set up to work from home, Lapidus has equipped them with iPads and certain types of equipment needed at home, along with the necessary training to use them. Staff are provided with protocols on how to shift to working at home and about what is expected to happen between them and their clients. “We’re coming up with remote work policies,” she said.
Large gatherings have been canceled, of course, such as regular community education programs. “We are trying to abide by no large gatherings of more than 10 people,” said Lapidus.
They also plan to continue with their crisis care centers, which include 16‐bed units, she noted.
“We have an urgent recovery center and bed unit for the most vulnerable persons who are a danger to themselves and others. Providing those types of services cannot be done virtually, That operation is still active.” – Gail Lapidus
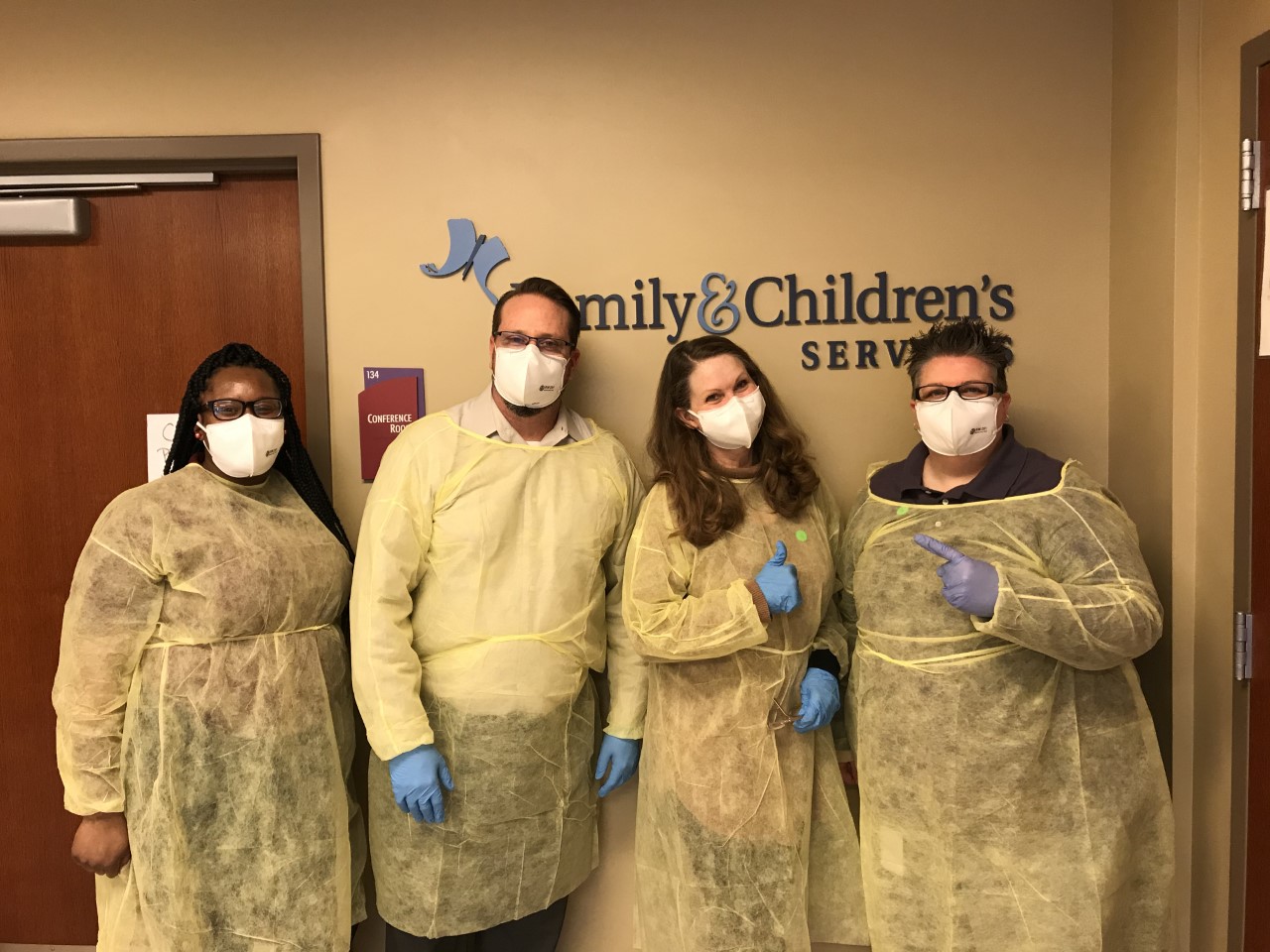
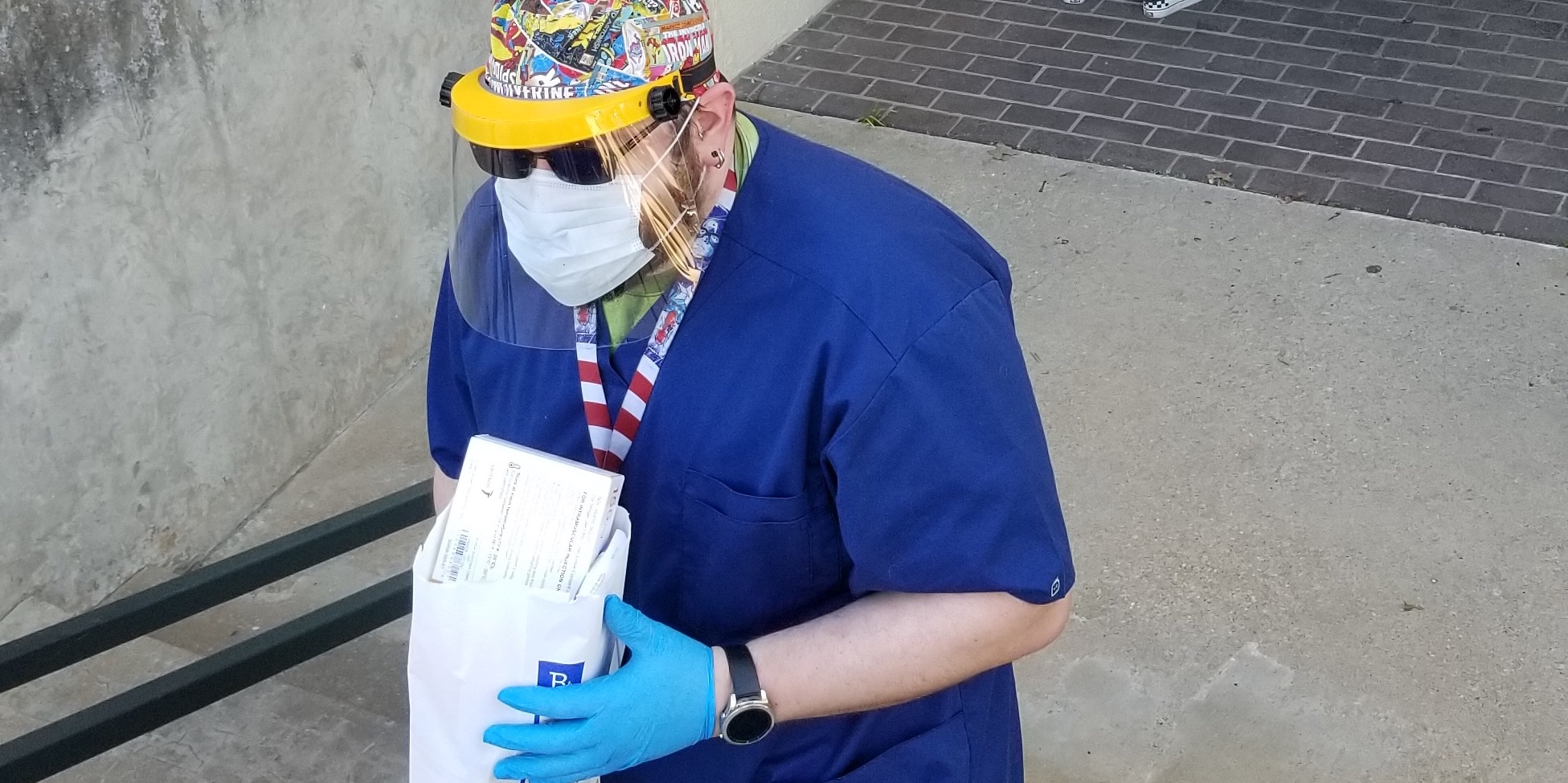
Safety is an important issue no doubt for staff at the recovery center, she noted. “We’re trying to get protective gear,” she said. They are awaiting approval for an N95 mask, which is fairly guaranteed to keep infections out, said Lapidus. They also are in short supply of face shields, she said. Employees are reminded to be careful. “We’re dealing with a vulnerable population that might be contagious,” she said. “We don’t know.”
“If you’re seriously sick, you’re going to need to be in the hospital,” Lapidus said. “The big concern in the country is if we will have enough beds for the most seriously ill.”
Dealing with the needs of the homeless population is also challenging, she noted. “They have no home to go to if they get sick,” Lapidus said. However, she added, “What is a safe place where they can be quarantined?”
Prolonged isolation
Lapidus expressed concerns about the effects of prolonged isolation on children, families and the elderly as “we are moving away from gyms, churches, recreation centers, playdates, yoga, bars and typical activities one engages in for relief from stress and anxiety.” Gatherings of teenagers have also stopped, she said. “This is affecting every single stage of life,” said Lapidus. “It’s all been taken away in one swoop.”
“I worry about what effect it will have on people. Tempers are flaring; there’s concern of domestic violence and child abuse increases during this isolation. There are also more chances of more depression and suicides rising.” – Gail Lapidus
In response, Lapidus has prepared public care reminders, urging people to use apps or talk to family members, for example. “We’re trying to build up what we call in the field ‘protective factors,’ against this uncertainty that we don’t know when it will end,” she said.
She has also created a team to come up with ideas and information that can be sent to clients, including suggested therapies and treatment plans. Having conversations with clients is important. Clients may feel depressed and scared, she noted. “We have to do a little bit more preparation in the volatility that might happen in mood or behavior,” she said. She’s advising staff to start scanning the literature, sending out apps for people to use to cope with stress, and sending guidance from the mental health field. “People are being locked up at home; that’s a risk factor,” Lapidus said.
“I send out a daily coronavirus update to my employees,” she said. “It’s important to engage with employee groups as frequently as they can so there’s not a vacuum of information.” Lapidus sends daily emails to staff and copies the correspondence to the board.
Telehealth/Teletherapy
Family & Children’s Services delivers some of its telehealth services in a virtual environment, Lapidus said. The services are provided by doctors or psychiatrists. “Our clients with serious mental illness found it to be as effective as face‐to‐face” communication, she noted. Lapidus said she hopes that moving forward with teletherapy services will be just as positive.
Clients have not experienced teletherapy before, having been accustomed to services being delivered in a physical setting, she said. This is different, she noted. “It’s on a massive scale to have all of the therapists working from home and providing teletherapy services,” she said. “It’s going to be a big leap for providers and the people we serve.”
“This is affecting every single stage of life. It’s all been taken away in one swoop.” – Gail Lapidus








